Are there specific inflammatory markers or pain signaling pathways that are activated in the knee joint during walking but not the other activities?
GPT o1 answer:
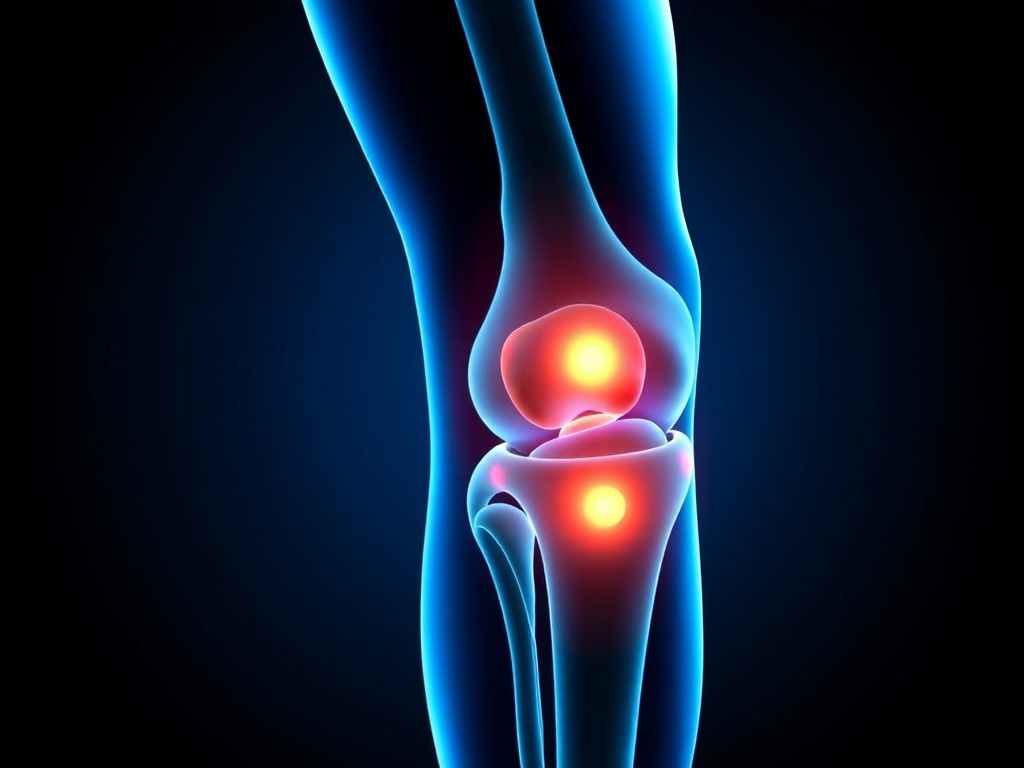
Yes, there are specific inflammatory markers and pain signaling pathways that can be activated in the knee joint during walking but not as prominently during activities like swimming, rowing, or biking. This is primarily due to the weight-bearing nature and higher mechanical stress involved in walking, which can exacerbate underlying joint issues and trigger inflammatory responses.
Inflammatory Markers:
-
Pro-inflammatory Cytokines:
-
Interleukin-1β (IL-1β) and Tumor Necrosis Factor-alpha (TNF-α): These cytokines are key mediators of inflammation and are often elevated in conditions like osteoarthritis. Mechanical stress from walking can stimulate their production in the knee joint.
-
Interleukin-6 (IL-6): Elevated levels of IL-6 are associated with joint inflammation and pain. Weight-bearing activities may increase IL-6 secretion compared to low-impact exercises.
-
-
Matrix Metalloproteinases (MMPs):
-
MMP-1 and MMP-13: These enzymes degrade collagen in cartilage. Increased mechanical loading during walking can upregulate MMP expression, leading to cartilage breakdown and pain.
-
-
Prostaglandins:
-
Prostaglandin E2 (PGE2): This lipid compound contributes to inflammation and pain sensation. Walking-induced stress can enhance PGE2 synthesis in the knee joint.
-
Pain Signaling Pathways:
-
Mechanical Stress Activation:
-
Ion Channels (e.g., TRPV1, ASICs): These channels on nerve endings respond to mechanical stress. Walking can activate these channels, leading to pain signals that are less triggered during non-weight-bearing activities.
-
-
Nerve Growth Factor (NGF):
-
NGF is involved in sensitizing pain fibers. Increased mechanical load during walking can elevate NGF levels, enhancing pain perception in the knee.
-
-
Substance P and Calcitonin Gene-Related Peptide (CGRP):
-
These neuropeptides are released from sensory nerves during stress and contribute to vasodilation and inflammation. Their release can be higher during walking due to greater joint stress.
-
Why Walking Affects Inflammation Differently:
-
Weight-Bearing Load: Walking imposes a significant load on the knee joint, increasing mechanical stress on cartilage, ligaments, and bone. This can lead to micro-injuries or aggravate existing damage, prompting an inflammatory response.
-
Joint Alignment and Gait Mechanics: Abnormal gait or joint misalignment during walking can concentrate stress on specific areas of the knee, leading to localized inflammation and pain.
-
Reduced Muscle Support: If certain muscles are weak, the knee may not be adequately supported during walking, increasing joint stress and activating pain pathways.
Contrast with Swimming, Rowing, and Biking:
-
Low-Impact Nature: These activities are low-impact and involve minimal weight-bearing on the knees, reducing mechanical stress and the consequent activation of inflammatory markers.
-
Continuous Movement Without Impact: The fluid motions in swimming and cycling promote joint mobility without the repetitive impact loading that occurs during walking.
-
Muscle Engagement: These activities often engage different muscle groups more evenly, providing better joint support and reducing the likelihood of stress-induced inflammation.
Clinical Implications:
-
Diagnostic Biomarkers: Elevated levels of specific inflammatory markers during walking could serve as biomarkers for diagnosing knee pathologies associated with mechanical stress.
-
Targeted Therapies: Understanding these pathways allows for the development of treatments aimed at inhibiting specific inflammatory mediators activated by weight-bearing stress.
-
Personalized Exercise Programs: Individuals with knee pain may benefit from low-impact exercises that maintain joint health without triggering inflammatory responses.
Conclusion:
Walking can activate specific inflammatory markers and pain pathways in the knee joint due to the mechanical stresses involved. These responses are less pronounced during low-impact activities like swimming, rowing, or biking, which do not impose the same level of weight-bearing stress on the knees. Recognizing these differences is crucial for managing knee pain and developing effective treatment and rehabilitation strategies.